COVID-19 is no longer officially a global health emergency, but the World Health Organization (WHO) says SARS-CoV-2, the virus which leads to COVID-19, is here to stay.
New booster shots designed to target omicron subvariant XBB.1.5, which is currently the most dominant, are expected to become available by September or October — at the start of autumn in the Northern Hemisphere.
Boosters will be offered to people over 65 and those with illnesses that put them at risk.
However, there are concerns that existing vaccines will be ineffective against emerging strains like EG.5, also known as Eris.
When should I get my next COVID booster vaccine?
On August 9, 2023, the WHO classified EG.5 as a "Virus of Interest," one step below the more serious level of "Virus of Concern."
That so-called "risk evaluation" for EG.5 seemed to prompt a New York Times article to suggest readers would be "a lot better off" if they waited "another month or two" to allow for an updated vaccine to be approved instead of getting whichever boosters were available now.
Further down, their advice — based on interviews with three US-based infectious diseases and vaccine experts — appears a little confusing.
First, they say that "antibodies produced by the updated vaccine may not be quite as effective against [EG.5]." Then, they say, "The new booster is still a better fit for EG.5 than last year's booster."
So, should you or shouldn't you get a booster vaccine now?
Waiting to get a booster is 'silly advice'
The experts DW contacted for this article challenged the advice in the NYT, arguing that any vaccine was better than none, especially if you are older than 65 years or have a condition that puts you at risk of severe COVID-19 symptoms.
"This is silly advice," said Paul Hunter, an emerging infectious disease expert at the University of East Anglia, UK. "It's better to have the current vaccine than wait for an improved one."
Wait for a new vaccine, said Hunter, and you increase the risk of serious COVID-19 infection from a current variant.
"Every new variant that has appeared since omicron hangs around for three months. If you wait a few months before getting a[n updated] vaccine that's good against EG.5, the variant will be history by the time the vaccine comes to market," Hunter said.
What is the best COVID vaccination strategy?
COVID is currently being managed by seasonal vaccination programs.
"We don't have a long-lasting or sterilizing vaccine like we do for measles. Therefore, immunity doesn't last from year to year," said Keith Neal, an epidemiologist at the University of Nottingham, UK.
We must rebuild immunity for each new COVID variant through infection or booster shots.
Vaccines can be changed quickly to target the latest coronavirus strains, so they are always catching up with new variants.
The difficulty with developing new shots is knowing which strains will likely be the most dominant in the coming months.
"It's similar to the flu vaccine, where we make an informed guess — we say, 'Look, this variant has been circulating in Australia this winter, so we'll put that in our vaccine for the Northern Hemisphere's upcoming winter,'" said Neal.
Neal said the best strategy is to get your COVID-19 vaccine whenever you can.
"If things change substantially, we could give high-risk people a second COVID booster this winter. We always have strategies for situations that go worse than expected," he said.

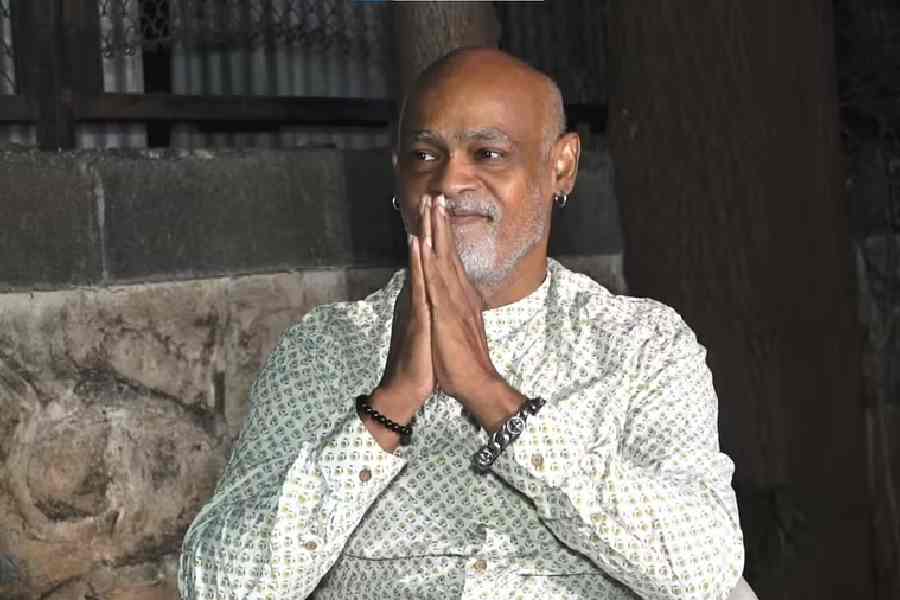
People over the age of 65 and those with conditions that cause greater risk of severe COVID-19 will be offered COVID-19 boosters Deutsche Welle
Why vaccinate in autumn?
Respiratory virus infections, such as COVID-19 and influenza, tend to be more frequent in winter than in summer and also tend to cause more severe diseases.
Timing a booster campaign to early autumn gives the best protection during the worst time of the year for respiratory viruses.
"It means you can reduce COVID infections at a time when other respiratory infections are quite high, which takes pressure off health services. Getting both influenza and COVID at the same time isn't good," said Hunter.
Vaccines don't necessarily reduce virus transmission from one person to another, said Hunter, but they do protect people against severe infections.
"It does this very well, especially in people with hybrid immunity — that is, immunity from vaccination and a prior COVID-19 infection. This is why it's so important to get vaccinated," Hunter said.
Is there an alternative to seasonal COVID vaccines?
Moderna, a US-based pharmaceutical company, published early trial dataon August 17 that suggested their new mRNA COVID vaccine targeted XBB strains and was effective against EG.5 and another emerging variant called FL1.5.1 or "Fornax."
At the time of writing, their updated vaccine was awaiting approval by the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA).
While this is good news for booster programs in the short term, it does little to establish long-term sterilizing immunity, and some worry that vaccine fatigue may hinder such long-term immunity.
So, scientists are working on a pan-sarbecovirus vaccine — a vaccine that causes long-lasting and universal sterilizing immunity to SARS-CoV-2, much like the shot that helped eradicate smallpox.
"This wouldn't just work against SARS-CoV-2, but also against other beta coronaviruses, meaning it would be hugely beneficial against future potential pandemics," said Hunter.
Promising pan-sarbecovirus vaccine candidates are in the works, but substantial development costs hinder progress. The first candidates may come into clinical use in 2024.