Sarah Teichmann, co-founder of the Human Cell Atlas (HCA), was in Calcutta to deliver a talk on mapping the human body. She and Partha P. Majumder, past president of the Indian Academy of Sciences in Bengaluru, spoke about HCA and gene mapping, the technology involved and how it will translate to public life with Prasun Chaudhuri on the sidelines of the event. Here are excerpts from their conversation.
PC: What do you want to achieve by drawing up a map of all the cells in the human body?
PPM: You mean the mission of the HCA?
ST: We are working to create comprehensive reference maps of all human cells as a basis for understanding human health and for diagnosing, monitoring and treating diseases.
PPM: You mean an atlas mapping which genes are expressed in which cells of the body. Is that right?
ST: Yes, that and also where each cell is located
in relation to other cells in an organ.
PC: How did you come to be interested in this giant project?
PPM: If I am not wrong, Azim Surani’s early study of five individual cells of the mouse embryo influenced the formation of the HCA.
ST: Yes, the publication from the Surani lab in Cambridge University in 2009 was the first example of single cell genomic profiling of cells. It proved that it is possible to sequence all expressed genes inside a single cell, and heralded the resolution revolution in genomics. The technology developments in single cell and spatial genomics meant that by 2016 it was clear that a project like the HCA was feasible.
PC: How many genes are there?
PPM: About 20,000 genes are encoded in the DNA of each cell. These are chemically transcribed into the RNA and then as proteins. Sarah, how do you measure expression levels of genes in a single cell? (Gene expression level refers to the volume of gene transcription produced in a cell.)
ST: The basic method is to dissociate and collect single cells using a tube of a very small diameter and then carry out next-generation sequencing of tiny volumes of DNA. High-resolution microscopy for simultaneous detection of thousands of molecules in individual cells in thin tissue sections has made spatial genomics possible.
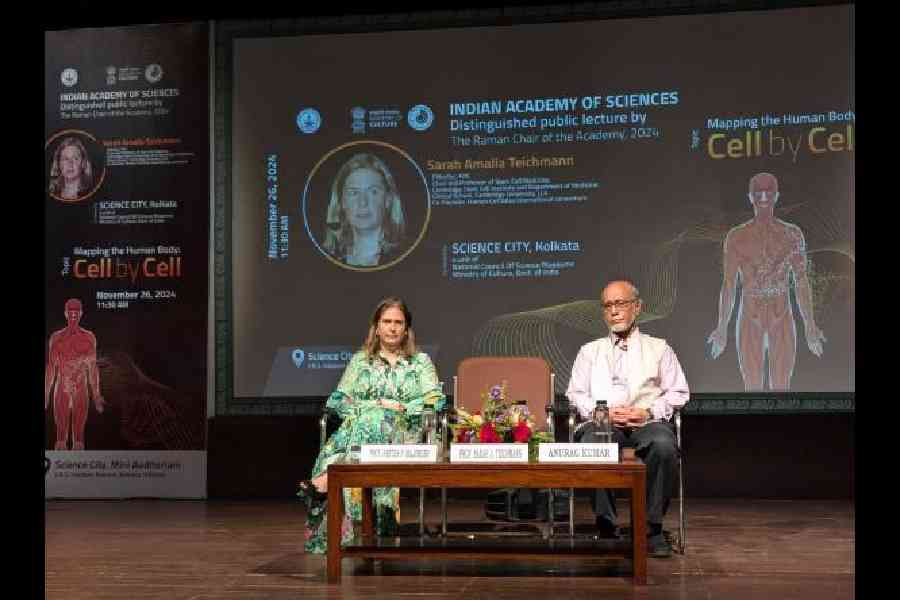
Sarah Amalia Teichmann in conversation with Partha P. Majumder Photo: Prasun Chaudhury
PPM: This endeavour must be technologically intensive. Did you and Aviv Regev (co-founder and co-chair of the HCA) play any role in the development of these technologies?
PC: HCA seems to be one of those rare global projects headed by women…
ST: Yes, both of us, as well as many others in the community, contributed to the optimisation of the single cell and spatial genomics technologies, and also the procedure for computational analysis of the vast amounts of data produced by these methods.
PPM: After identifying which genes are expressed
in which tissues, how do
you determine the type of that cell?
ST: A combination of human and artificial intelligence is involved in determining it.
PPM: Has the HCA research identified any new types of cells?
PC: You mean there have been discoveries?
ST: Yes, discoveries of new cell types and cell states is the most exciting part of this project. Not only have we found new cell states, such as innate T cells present in the human embryo, but also surprising new features of known cell types, such as hormonal regulation of pacemaker cells that determine our heartbeat.
PPM: Those participating in HCA research are only characterising cells from normal tissues. How will this help in identifying disease and providing treatment?
PC: So the map will work like a catalogue, to compare and contrast healthy and diseased cells?
ST: Yes, and this is incredibly useful for precision medicine and drug development. HCA data is being heavily used by pharma and biotech industries already.
And Partha, you have yourself been an active member of HCA research on the diversity of immune cells.
PC: Yes, how have Indian researchers contributed?
PPM: The human body contains cells that help us fight infections and develop immunity. The prevalence of infectious diseases is variable within and between populations. A consortium of researchers, including myself, is investigating the nature and extent of diversity in the cells of the immune system in healthy individuals drawn from different Asian populations using single-cell RNA technology. If we can understand this, we may be better able to understand why the prevalence of an infectious disease varies.
Sarah, meanwhile, has done seminal research on understanding the SARS-CoV-2 infection and the Covid disease.
PC: Will this research help us understand future epidemics better?
ST: In early 2020, the HCA community rallied to pool data and map the SARS-CoV2 viral entry factors. This showed the specific cells using which the virus enters through the eyes, nose and mouth. It was this knowledge that informed public health policies, such as masking up. Subsequently, we studied the immune response to the virus in the nose and blood of infected individuals, which provided important and interesting insights that will inform future epidemics or pandemics, drug development and vaccine design.
PC: You mentioned in your lecture that the HCA is also helping researchers understand preterm birth.
PPM: Birth before 37 weeks of pregnancy is a major problem.
ST: We have studied the placenta in detail. This has provided insights into the structure of the vasculature, immune system and genetic variants that can affect its development and, by extension, that of the foetus.
PPM: What is the HCA headed for in the future?
ST: In the coming years, we need to push forward the mapping of cells and release a more complete atlas. We also need to focus on data integration and making this data accessible.