Traumatic brain injuries affect millions of people across the world every year. This includes victims of falls or road accidents and soldiers or security personnel injured in the line of duty. Soon after such a serious blow to the head, there’s a cascade of immune responses that results in the swelling of the brain, which gets compressed in the skull. This often leads to a life-threatening condition.

The IISc team collaborated with neurosurgeons at M.S. Ramaiah Medical College in Bangalore to place the 3D printed bone flaps on the skulls of 10 patients through cranioplasty Sourced by The Telegraph
To relieve the pressure on the brain, a neurosurgeon usually removes a slice of bone from the skull — a procedure known as decompressive craniectomy — to give the swelling brain room to expand. When the injury has healed sufficiently and the inflammation has subsided, the opening in the skull is surgically patched up, if possible with the removed bone that was preserved in a sterilised environment.
Reconstructive surgery to treat the craniectomy defect is known as cranioplasty. In the late 19th century surgeons started using bone grafts, usually sourced from the patient’s body, for cranioplasty. Unfortunately these did not readily conform to many three-dimensional defects and had an unacceptable cosmetic appearance. The immune reaction and other complications in the grafts encouraged surgeons to experiment with metals or synthetic materials while treating soldiers injured in the two world wars.
In recent times, a plate or mesh made of titanium, a malleable and non-corrosive metal, has been commonly used as implants in cranioplasty. A neurosurgeon grafts a piece of the metal or mesh to replace the missing bone. However, these implants sometimes cause delayed wound complications and erosion through skin. Above all, the metallic implants are expensive.
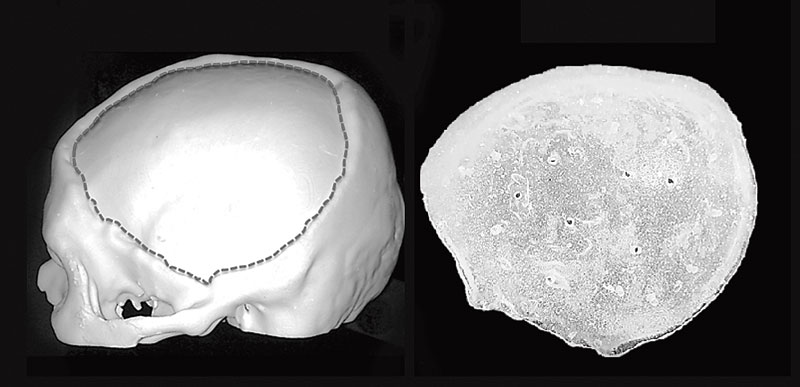
The IISC team printed this 3D model of a defective skull and (right) the acrylic flap that was used to mend it Materials Research Centre, IISc
Among synthetic materials, polymethyl methacrylate (PMMA), an acrylic glass, has emerged as the ideal material for skull implants in the last few decades. Also called PMMA bone cement, the material is inexpensive, strong, light, non-reactive and stable. Moreover, it is an inert biomaterial that does not cause an inflammatory reaction, there are no known allergies to it and it is not rejected by the body. That is why the US Federal Drug Administration has approved it as a prosthetic implant for hip, knee and other joint replacements.
But using PMMA implants is a complex procedure; the material has to be manually shaped and fixed in place of the missing bone by the surgeon. It is a challenge to place the implant properly before it hardens and PMMA hardens quickly.
Now Bikramjit Basu, a materials scientist at the Indian Institute of Science in Bangalore, has innovated a method that may make the whole process simpler and quicker. It customises the PMMA implants using a model of the defective skull fabricated using 3D printing, a technology used to make three-dimensional objects based on digital images. The 3D printing of body parts is gaining ground all over the world (see Print on demand). Says Basu, “Before making a cast of the implant, we take CT scan images of the patient’s skull and reconstruct a model of the cranium, delineating the contours of the defect of the skull.”
The printing of the cranium model is then done in a unique binderjet printing process protocol, innovated by the IISc team. The technique employs inkjet printing technology — which dispenses a binder, droplet-wise, onto a powder and leaves a solid body behind — and the entire model is printed layer by layer. The fabrication process follows the contour or design profile generated by a computer-aided design of the skull defect. “The importance of 3D powder printing lies in its ability to fabricate a patient-specific model of the cranium with complex defect morphology at room temperature using a binder,” says Basu.
The patient-specific 3D implants have a better anatomic fit and more satisfying aesthetic results than any other implants. It is able to resist pressure inside the cranium and has enough elastic strength. The synthetic bone flaps created by the IISc team are undergoing clinical trial.
The IISc team collaborated with neurosurgeons at M.S. Ramaiah Medical College in Bangalore to place the 3D printed bone flaps on the skulls of 10 patients through cranioplasty. It has now been over a year and all 10 patients have fully recuperated, showing accurate restoration of the symmetrical contours and curvature of the cranium. The neurosurgeons who headed the team, Dr Aniruddha Jagannatha and Dr K. Khanapure, now work at Vikram Hospital in Bangalore. Inspired by their earlier success, cranioplast implants are currently being clinically tested at the Datta Meghe Institute of Medical Sciences in Wardha, Maharashtra.
The success of cranioplast implants by the IISc scientists and their clinical collaborators is a significant step in the domain of reconstruction surgery in India. The use of 3D reconstruction techniques from medical images could reduce the possibility of errors during surgery, offer an improved fit and provide implant stability. It reduces surgery time in complicated procedures such as cranioplasty and has better clinical outcomes.











