I have a lot of pain during periods — it is always such an uncomfortable, unpleasant experience. It often seems like my friends and others around me are not suffering as much as me, and I am not sure what to do sometimes to deal with it!
— Hurting Harshita
Dear Hurting Harshita,
I’m so sorry to hear you are having unpleasant, painful periods. Even if your friends aren’t always vocal about their discomfort, at least 84 per cent of people who menstruate experience period pain, and 43 per cent experience it every period. It can be an isolating experience to be in pain, particularly when it is severe. This World Menstrual Hygiene Day, let’s dive into the topic of dysmenorrhea or menstrual pain.
In general, periods cramps occur because of hormone-like substances called prostaglandins that create contractions in the uterus that help squeeze out blood from the uterus much like your average lime squeezer (even if this doesn’t make for the best nimbu pani).
How to know if your pain is a ‘normal’ level
If your pain is at a level where it is mild to a level where it doesn’t disrupt your life, or occurs infrequently, then you may not need to worry. However, if you’re experiencing pain every cycle which is severe, doesn’t go away with quick home remedies, or is making you faint, you may need to see a doctor.
Severe pains can mean that you have an underlying condition like uterine fibroids, endometriosis, adenomyosis, pelvic inflammatory disease and cervical stenosis. Doctors may recommend tracking your period symptoms, getting an ultrasound on a certain day of your cycle, and then accordingly prescribe a course of action.

Severe pain during periods that doesn’t go away with quick home remedies, or is making you faint, may indicate an underlying condition Shutterstock
Unfortunately, most of medicine has invested little in investigating specific causes and cures of “women’s” reproductive health issues. For instance, while a whopping 10 per cent of people assigned female at birth have endometriosis, we still don’t know how to definitively cure it — it also takes an average of 8-12 years for cis women to get a diagnosis of endometriosis. Partly because it can be difficult to detect, and partly because of doctors not taking women’s pain as seriously. Personally, my endometriosis diagnosis came after months and years of “clear” ultrasound reports. Please don’t ignore your severe pain!
Period pain sucks, but you can make it suck less
While you’re on your period, you can use a few simple strategies to help you cope with painful symptoms. Different ones may work for you, I tend to use a combination of a few methods:
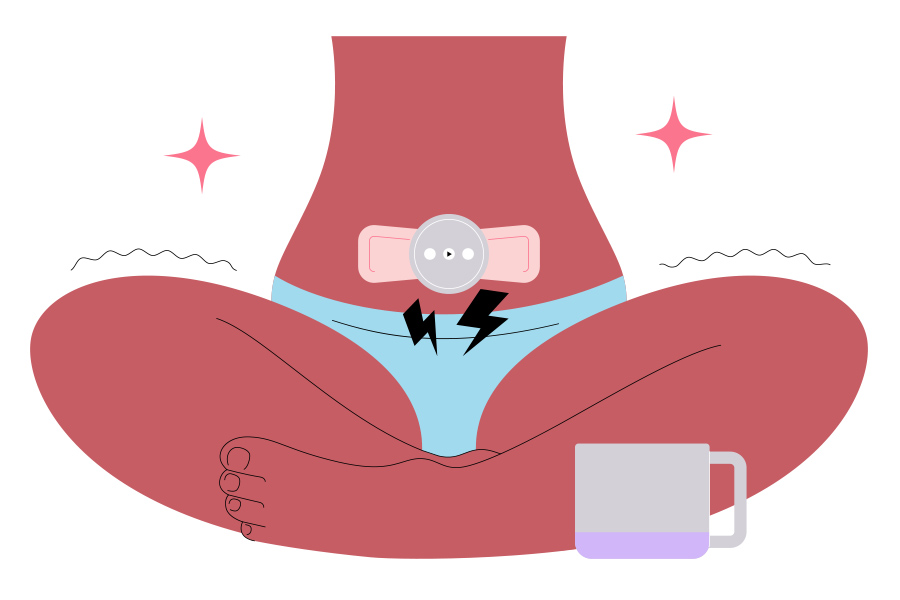
- Immediate comfort through warm compress: Like a hug on a cold day, a warm compress can provide immediate relief and comfort. You can use an old-school hot water bottle, an electrical heating pad, or even take a warm bath or shower. If you’re on the go, you can also consider trying heat patches specifically designed to combat menstrual cramps, such as the heat patches from Sirona and Carmesi.
- Massage and movement to boost circulation: A gentle massage if you’re having leg pain, head pain, or back pain, and even a bit of yoga, a gentle walk and movement can help dramatically reduce pain by boosting circulation. While you may want to roll into a ball in bed, stretching out and creating motion could actually be more helpful.
Shutterstock
- Painkillers can redeem your day: There is so much stigma and hesitation around the use of painkillers for periods, including myths around becoming infertile or harming the uterus. However, many doctors say that some monitored painkiller use — a couple of times a month — is okay to manage your menstrual pain. Different types of painkillers may provide you better relief depending on your types of pain. Paracetamol may work for general pain relief, ibuprofen for inflammation-based pain (if you have endometriosis, for example) or an antispasmodic specifically for muscle cramps in the uterus. Talk to your gynecologist about your options.
- Use a topical CBD oil roll-on for pain relief: Topical roll-ons are great especially for milder pains. You can also use them in combination with other methods. I like using my roll-on in the 30-minute wait for my painkillers to kick in. You can buy these easily from a number of brands — I like the ones from Bombay Hemp Company and India Hemp Organics.
Rearrange your life to support your cycle
Fundamental long-term life changes, while difficult to implement, can go a long way in supporting your cycle. These changes can dramatically change the way you experience your cycle, even if you practice them intentionally 7-10 days before your period each month.
- Slow down, get some extra Zs: If your period has a roughly predictable schedule, or you start to experience PMS symptoms, start to plan your life around slowing down and getting some rest. Advanced moves would even be to schedule big meetings, work deadlines and vacations based on the approximate timing of your period.
- Move according to your cycle: Some fitness coaches recommend syncing your cycle to how you work out. Reserve big, intense strength training for the first 7-10 days after your period. After ovulation (roughly day 14 for a 28-ish day cycle), you can start winding down and focus more on mobility, gentler movements, take a longer time for recovery.

Fundamental long-term life changes can go a long way in supporting your cycle Shutterstock
- Eat less inflammatory foods: Changing the way you eat can be a difficult, but important way to support your cycle. It can especially be hard when you’re feeling emotionally and physically drained, so only do this as much as you are able to manage easily. I’ve found it helpful to at least cut back a little bit (even if not completely) on foods that can cause inflammation (sugar, salt, processed foods, fried foods, wheat, dairy) and eat more anti-inflammatory foods (fruits, leafy greens, nuts). If you can’t manage it through the whole cycle, even seven days each month can be helpful.
- Manage mental health and stress: Stress and poor mental health can also exacerbate your pain symptoms. Prolonged emotional stress can lead to a lot of fluctuations in the menstrual cycle. Meditate, speak to a therapist, and do the things you need to do to manage stress.
All in all, periods can be uncomfortable, but there are ways to chip away at that discomfort. Lastly, and I repeat, please please see a doctor if your pain is something that is interfering with your life. Severe, life-disrupting pain is not normal. All the best, and hope you feel better soon!
Karishma Swarup is a Kolkata-born and raised sexuality educator, Instagrammer (@talkyounevergot) and works at a global consulting firm. She busts myths about sex, pleasure, intimacy, orgasms, periods, and all things related to sexual health.
If you have a question you would like Karishma to answer, send an email on mykolkata@telegraphindia.com with the subject line ‘Questions for Karishma’ or DM/comment on our Facebook, Instagram, or Twitter.


