India by early May already had over 6.4 million people infected with the new coronavirus, the national health research agency said on Thursday, estimating an epidemic size about 100-fold higher than counted through lab-confirmed cases.
The Indian Council of Medical Research (ICMR), releasing detailed findings of the first nationwide household survey for the coronavirus, has estimated that for every lab-confirmed diagnosed case, India has 82 to 130 undocumented coronavirus infections, depending on the location.
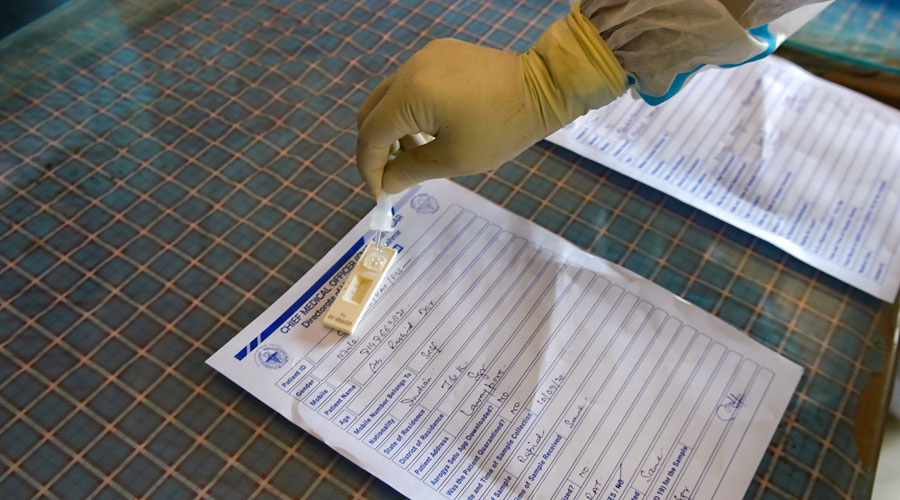
(During the day, the Union health ministry directed states to ensure that symptomatic patients who test negative on an “antigen” test for the coronavirus infection are retested with a confirmatory viral test amid concerns that the infection could spread without retests.
The directive follows concerns that in some large states, symptomatic patients found negative through the relatively less reliable rapid antigen tests (RATs) are not being followed up by the more reliable confirmatory RT-PCR tests, the health ministry said.)
The nationwide household survey that screened 28,000 persons from randomly selected households in 70 districts or cities across India found the infection prevalence ranged from 0.68 per cent to 1.03 per cent, with an overall nationwide prevalence rate of 0.73 per cent.
The findings suggest a cumulative 6,468,388 adult infections by early May, Manoj Murhekar, director of the ICMR’s National Institute of Epidemiology, and his collaborators said, describing their findings in the Indian Journal of Medical Research.
The survey from May 11 to June 4 looked for antibodies that indicate previous exposure to the infection.
Health authorities across the country had by May 8 detected 59,662 lab-confirmed cases of the coronavirus disease. The estimate of over 6.4 million actual infections points to a silent and undetected spread of the infection long suspected by public health experts.
The high infection-to-case ratio in India may be due to the “prioritisation of testing among symptomatics and variability of testing rates across states”, the researchers said.
Public health specialists had in the early months of the epidemic expressed concern that narrow testing strategies would miss many people infected as 80 per cent of infected persons have no symptoms or only mild symptoms.
The survey has estimated that the infection fatality rate — the proportion of deaths among the total number of infections — in India ranged from 0.18 (0.0018 per cent) in districts with least prevalence to 11 (0.11 per cent) per 10,000 infections in districts with the highest prevalence on May 24. The numbers changed to 0.27 (0.0027 per cent) to 15 (0.15 per cent) on June 1.
In comparison, India’s case fatality rate — the proportion of deaths among lab-confirmed Covid-19 cases — is 1.7 per cent.
The IFR in India, the researchers said, appears lower than documented in other countries — such as 0.12 per cent in the US or 1 per cent in Brazil and Spain.
But the ICMR researchers cautioned that their IFR estimate is likely an “underestimate” because of incomplete death reporting and lack of access to testing facilities required to confirm Covid-19 deaths.
The ICMR has since embarked on a second nationwide survey in the same districts whose results are expected to be analysed later this month. “A second survey in the same locations would allow us to assess how the infection prevalence has changed in three months,” a survey team member said.
The IFR, the researchers have pointed out, represents the “societal cost” of achieving herd immunity to SARS-CoV-2, the virus that causes Covid-19, through infections.
Herd immunity is a phenomenon under which a viral infection has spread to such a large proportion of people that the infected persons themselves pose a barrier to further spread of the virus.
Some medical experts have estimated that herd immunity against SARS-CoV-2 would require roughly 60 per cent of a population to be infected, although there is still uncertainty about this number.
Retest
The Union health ministry explained why it directed states to ensure that symptomatic patients who test negative on an “antigen” test for the coronavirus infection are retested with a confirmatory viral test.
Retesting is necessary to ensure that such symptomatic negative cases on antigen tests do not spread the infection among their contacts, the health ministry and the ICMR said in a joint letter to all states and Union Territories.
The antigen tests, which look for tiny chunks of viral proteins, are less expensive and can yield results within 30 minutes, but also come with significant proportions of “false negative” results — a condition in which an infected patient is labelled as negative.
The ICMR’s testing strategy, recognising this potential for false negative results, had asserted that all patients with symptoms of cough, fever or breathlessness who test negative on RAT (rapid antigen tests) should be tested again with RT-PCR, a more reliable test that looks for viral genetic material. It had also recommended that asymptomatic negative cases of RAT who develop symptoms within two or three days of testing should also be retested with RT-PCR.
While the guidelines state the need for retesting, accounts from some states suggest not all symptomatic negative antigen cases are retested. Public health experts suspect the gaps in retesting might be the outcomes of either poor capacity or fatigue or a mix of both.
“The numbers we’re seeing today makes testing all contacts and symptomatic people logistically cumbersome and challenging,” said Oommen John, a public health specialist at The George Institute of Global Health, New Delhi.
India on Thursday recorded 95,903 new Covid-19 cases, raising the total number of infections to over 4.46 million of whom over 3.47 million have recovered, over 919,000 patients are under medical supervision and 75,062 have died. The average daily increase over the past seven days was 87,000 cases.
Under health ministry guidelines, states are expected to trace and test all direct contacts of 80 per cent of new Covid-19 cases within 72 hours of their diagnosis. Public health experts point out that even if each new Covid-19 patient had three contacts, health staff would need to test more than 250,000 contacts daily.
The Indian Public Health Association had last month urged the government to tweak the testing strategy to focus on patients with symptoms, cautioning that the current policy could lead to fatigue among health staff.