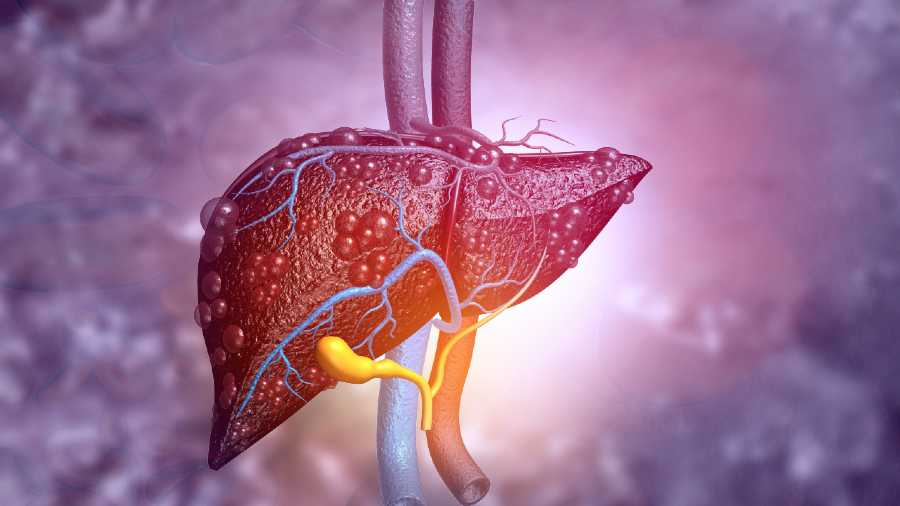
The liver is situated on the right upper part of the abdomen. It is essential for survival. All the blood from the stomach and intestines passes through the liver, where it is filtered — the toxic chemicals are removed and excreted from the body via the faeces. In addition, it produces bile (needed for digestion), makes proteins, regulates amino acids, helps control blood glucose levels and also regulates blood clotting.
The liver can get damaged and start to fail in its functions. The damage can be acute or chronic. Acute failure can occur due to an overdose of medications. Paracetamol is high on that list. It is available without a prescription and is used for fever, headaches and several other aches and pains. Children can take 10-15mg/kg/dose. This can be repeated every four hours. For adults, 2gm/day — 500mg every six hours — is the maximum recommended dose.
Other non-steroidal anti-inflammatory agents, some antibiotics, statins and anticonvulsants can also be dangerous. Herbal supplements from natural sources, such as aloe vera, may appear safe but the dosage is not scientifically titrated. They can react with allopathic medications. Wild mushrooms, insecticides and chemicals like carbon tetrachloride are other offenders.
Acute damage can occur from viral infections such as Hepatitis A, B, C, the Epstein-Barr virus, cytomegalovirus and the herpes family of viruses. Cancer, shock and heatstroke can also severely damage the liver.
By far, the commonest cause of slow and long-standing damage to the liver is alcohol. It causes inflammation, scarring and distortion to the liver anatomy so that it can no longer function normally. Moderate consumption — one drink a day for women and two for men — usually does not damage the liver unless there is an additional assault such as drugs or infection.
Non-alcoholic fatty liver can occur in people who do not consume alcohol. It tends to be more common in women. Risk factors include obesity, sedentary lifestyle, high cholesterol, non-insulin-dependent diabetes and bariatric surgery. It can result in extensive damage, cirrhosis and liver failure.
In the early stages, liver failure causes only a few vague or non-specific symptoms such as fatigue, pain and weight loss. So, it may be difficult to diagnose. As the liver continues to fail, fluid builds up in the abdomen, causing it to distend. This is called ascites. There may be prominent blood vessels on the shiny, stretched skin of the abdomen. The legs swell up. The muscles of the arms and legs waste away. The eyes turn yellow as unexcreted bilirubin levels build up. The distorted liver architecture causes venous blood vessels to swell in the oesophagus (varices). Vitamin deficiencies cause soreness of the tongue and the angles of the mouth. Anaemia may complicate the failure further.
Hepatitis A spreads through contaminated food and water. Hepatitis B spreads through contact with or the transfusion of contaminated blood. It can happen in case of unprotected sex with an infected person or the use of unsterilised needles. It can even spread from mother to her baby during childbirth.
Liver failure is diagnosed through blood tests, ultrasound, and CT and MRI scans. Confirmation may require a liver biopsy. Once the reason is confirmed, appropriate treatment can be administered.
Immunisation is available against Hepatitis A and B. Antiviral medication is available for Hepatitis B and C and also for herpes. Leptospirosis can be treated with antibiotics.
Alcohol consumption should be stopped immediately. It can worsen liver disease of any type. Sudden stopping may cause withdrawal symptoms with tremors and insomnia. These can be tackled with medication.
Alcohol dependency requires treatment with counselling and sometimes specific medications like acamprosate, disulfiram or naltrexone. These medicines cause unpleasant symptoms if combined with alcohol.
The writer is a paediatrician with a family practice at Vellore and the author of Staying Healthy in Modern India. If you have any questions on health issues please write to yourhealthgm@yahoo.co.in