Pancreatic cancer is a nasty, stubborn killer that has thus far defied medicine’s best efforts at early diagnosis and curative treatment. In November, it claimed the life of my friend Peter Zimroth, a 78-year-old New York City, US, attorney who was devoted to public service.
Zimroth was fit and active and in otherwise good health before symptoms developed — in his case, stomach pains and constipation. By that time, the cancer had spread and it was too late to operate.
Although pancreatic cancer is a relatively rare cancer, it is so deadly that it is now on track to become the country’s [the US’s] second leading cause of cancer-related deaths by 2040. Currently, it accounts for about 3 per cent of all cancers and 7 per cent of cancer deaths. Overall, only 1 in 10 people diagnosed with pancreatic cancer survives five years. A cure is almost always a lucky accident, when the cancer is detected at an early, symptom-free stage during an unrelated abdominal scan or surgery and the tumour can be surgically removed.
Dr Brian Wolpin, director of the gastrointestinal cancer centre at the Dana-Farber Cancer Institute in Boston, US, told me that this is such a hard cancer to find early because “it’s relatively uncommon in the population and the symptoms it causes, like weight loss, fatigue and abdominal discomfort, are nonspecific and more likely due to other conditions.” As a result, he said, “When 80 per cent of patients walk through my door for the first time, I know that we are highly unlikely to cure their cancer.”
Risk factors
Still, there are several major risk factors for developing pancreatic cancer. Smoking doubles the risk and accounts for about one-quarter of all cases. Being obese, gaining excess weight as an adult and carrying extra weight around the waist, even if not otherwise very overweight, also increase one’s risk.
That may be why type 2 diabetes — most often related to being overweight — is an important risk factor as well. Other risks include chronic pancreatitis, a persistent inflammation of the pancreas often linked to heavy alcohol consumption and smoking, and workplace exposure to certain chemicals, including those used in dry cleaning and metal work industries.
Older age is also a risk factor and family history may play a role too, including inherited genetic conditions such as mutations in the BRCA1 or BRCA2 genes that are most often associated with breast and ovarian cancers.
Warning sign
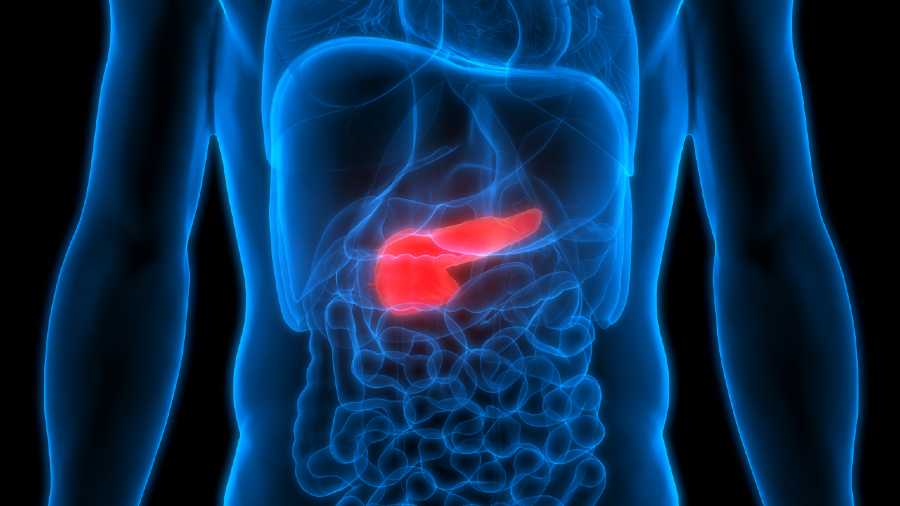
It has long been known that the best chance of surviving most cancers results from early detection, when the malignancy is totally confined to the organ or tissue in which it originates. (Blood cancers present different issues.) The pancreas is a rather small, carrot-shaped organ that lies well hidden between the ribs and the stomach.
An early cancer does not produce a lesion that can be felt, and it rarely causes symptoms that might prompt a definitive medical workup until it has escaped the confines of the pancreas and spread elsewhere.
But scientists are studying one possible early warning sign: a link between pancreatic cancer and newly developed type 2 diabetes. Diabetes, too, arises in the pancreas, which contains specialised cells that produce the hormone insulin that regulates blood-sugar levels. And although it’s not yet known which comes first, diabetes or cancer, some research suggests that the recent development of type 2 diabetes may herald the existence of cancer hidden in this organ.
An early study from 2005 of 2,122 residents of Rochester, Minnesota, US, by Dr Suresh Chari, now a gastroenterologist at the University of Texas MD Anderson Cancer Center, US, found that within three years of receiving a diagnosis of diabetes, people were six to eight times more likely than the general population to have pancreatic cancer. He, along with colleagues at the Mayo Clinic, also identified a gene called UCP-1 that may predict the development of this cancer in people with diabetes.
More recently, Dr Maxim Petrov, a professor of pancreatology at the University of Auckland School of Medicine, led a September 2020 study in New Zealand of nearly 1,40,000 people with type 2 diabetes or pancreatitis, or both, who were followed for up to 18 years. The findings revealed that those who developed diabetes after an attack of pancreatitis were seven times more likely to get pancreatic cancer than others with type 2 diabetes.
Another effort begun last summer by the Pancreatic Cancer Action Network, called the Early Detection Initiative for Pancreatic Cancer, will enrol more than 12,000 participants with elevated blood-sugar levels and new-onset diabetes. Half will have periodic blood tests and undergo abdominal imaging based on their age, body weight and blood-glucose levels to look for evidence of early pancreatic cancer, while the others will serve as controls.
NYTNS