A government analysis has bolstered suspicions that some private hospitals may have provided inappropriate treatment to sections of cancer patients to increase the amounts claimed under the nationwide health insurance plan.
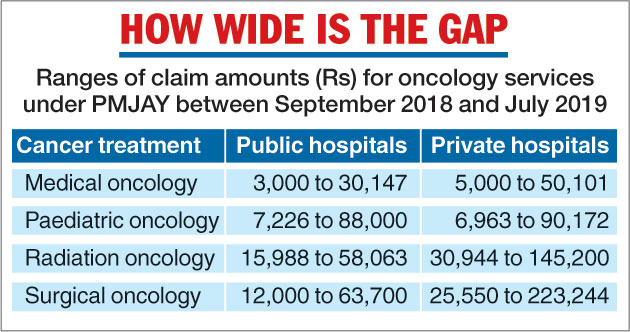
The paper, which examined the oncology services provided under the Pradhan Mantri Jan Aarogya Yojana, has found “stark variations” between the claims made by empanelled private and public hospitals. The private sector’s topmost claim figures for different types of cancer treatment were always significantly higher than the public sector’s. (See chart)
The Yojana, launched in September 2018 by Prime Minister Narendra Modi, pledges to pay the hospitalisation charges — up to Rs 5 lakh a year per household — incurred by 100 million poor households, which make up an estimated 40 per cent of the country’s population.
Public and private hospitals empanelled under the scheme can claim reimbursement for the services rendered.
The analysis, commissioned by the National Health Authority, which is implementing the Yojana, covered around 188,000 oncology-related claims made during the first 10 months of the scheme and found that 72 per cent were from private hospitals.
According to the paper, the higher average claim size from the private hospitals could be the result of higher treatment and surgeons’ charges or “provider-induced demand”, a term health economists use to describe treatment services encouraged by doctors or healthcare institutions.
“We’re only flagging some concerns — we cannot be sure that patients have received inappropriate treatment,” said Pramesh Chandra Bhatnagar, a medical doctor and the senior director, programmes, at the Voluntary Health Association of India, who had reviewed the paper.
“The average claims from the private sector are higher for the same sets of packages, which raises questions. But someone has to make a detailed patient-level analysis on individual claims to determine whether individual patients received correct treatment,” Bhatnagar told The Telegraph.
Health administrators in Maharashtra had intervened last year after noticing similar “higher-than-anticipated” oncology claims from some private hospitals, a state health official had told a special meeting of the Yojana in New Delhi earlier this year.
Sudhakar Shinde, a physician with the Maharashtra scheme that has been subsumed by the Yojana, said the state plan had observed private hospitals making claims for radiation oncology on unexpectedly large proportions of cancer patients.
“The packages under radiation oncology carry high reimbursements, and this raised suspicions whether some patients were being prescribed radiotherapy even though they may not have needed it,” Shinde said.
The state asked the empanelled hospitals to follow standard treatment protocols developed by the National Cancer Grid, a collaborative network of oncologists from the Tata Memorial Centre, Mumbai, and other hospitals.
Shinde said the standard protocols were only guidelines and that doctors were entitled to take decisions they felt appropriate for individual patients.
“But whenever deviating from standard protocols, doctors should provide a logical explanation of why they did so,” he told this newspaper.
In May this year, the Yojana signed a memorandum of understanding with the National Cancer Grid to promote uniform standards of care for prevention, diagnosis and treatment of cancer, among other things.
The analysis has recommended that cases be discussed with eminent experts involved with the National Cancer Grid to provide “treatment accordingly”.
It has revealed that oncology accounts for around 9 per cent of all claims and 30 per cent of tertiary-level claims under the Yojana. Maharashtra and Tamil Nadu were the highest “claim generators” for oncology services over the 10-month period.
The analysis also found that a skewed distribution of oncology services was leading to “major inequalities” in access to cancer care, with most patients still needing to travel long distances to receive treatment at premier hospitals.