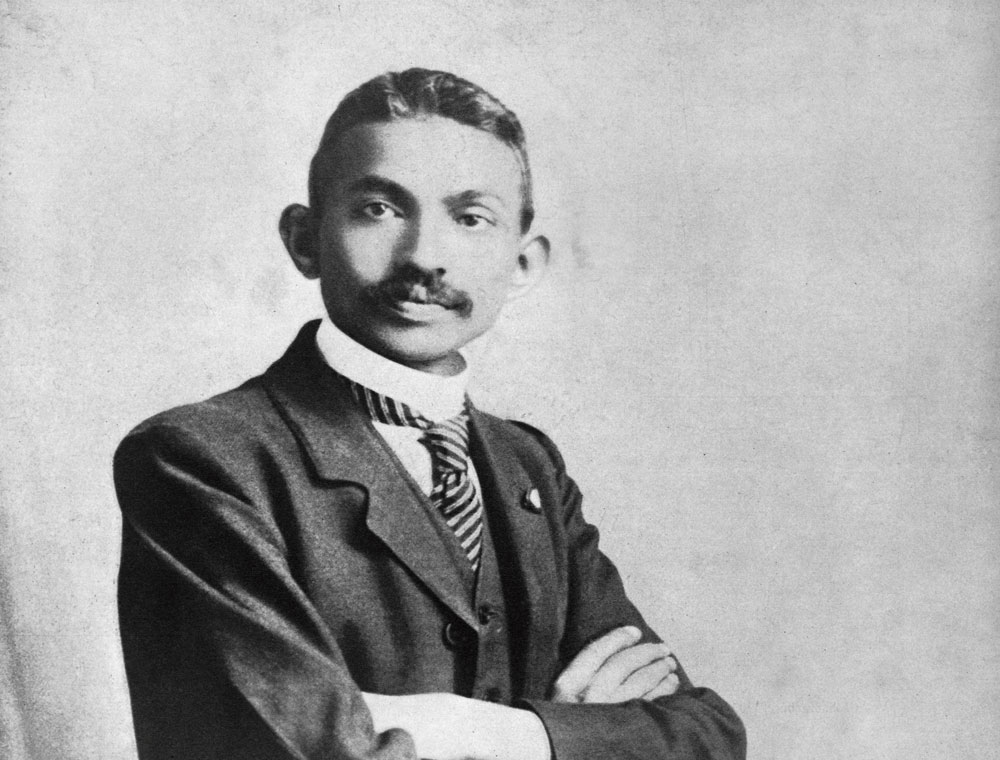
He was what they called in those days a “lampha” doctor. We are talking about Bengal of the late 1800s. The appellation lampha derived from Dr Sachindranath Sen’s LMF degree — he had passed the Licentiate Examination of the Medical Faculty from Calcutta’s Campbell Medical School. Lampha was also a reference to the oil lamp that was the constant companion of physicians those days, who roamed the countryside quite literally delivering healthcare from the wee hours of the day to deep into the night.
This story comes as a ragtag legacy; worn by telling and retelling in places, enhanced by creative memory in others. We are told that Sen was a classmate of Dr Bidhan Chandra Roy — genius physician-turned-chief minister of Bengal — at the Medical College, Bengal, from where he did his MB (bachelor of Medical Science) eventually. We are told how Sen didn’t join government service as the Boer War was on and his father did not want his young son enlisted. We are told that as a private practitioner travelling the length and breadth of India, he garnered first-hand knowledge of tropical medicine, especially diseases transmitted from animals to humans. We are told it was enough to turn him into an expert. And at some point, he was offered a position at the Calcutta School of Tropical Medicine; an offer he turned down as he was a hardened nationalist by then.
Researching tropical medicines, he contracted anthrax, and when he was cured, somewhat miraculously, he turned full-time private practitioner.
His patients were the people in his neighbourhood in south Calcutta, the domestic help, someone’s sister’s brother’s third cousin, someone else’s something else. The little garage space below the old apartment building that was his abode doubled as a laboratory for his compounder colleagues, Madhu Babu and Suleiman Vaid. This was also where he removed six-year-old Chutki’s tonsils.
He was an expert at reading the pulse and would often be summoned by some to call out the longevity of a terminally ill patient. He used to say he could see the aura of a patient as he felt the pulse kick away under his fingers.
The fee or compensation apparently did not matter. Some age-old family tradition, something to do with a family curse, prevented him from charging any. It is not sure how he ran his immediate family of five and extended family of more on these uncertain means, but it is believed that what the havenots couldn’t pay for was offset by thanksgivings from the haves. Someone would send home a week’s supply of rice, someone else the biggest brinjal from his garden, a Marwari patient once gifted him shares, another time he got some land from the Nashipur rajbari.
***
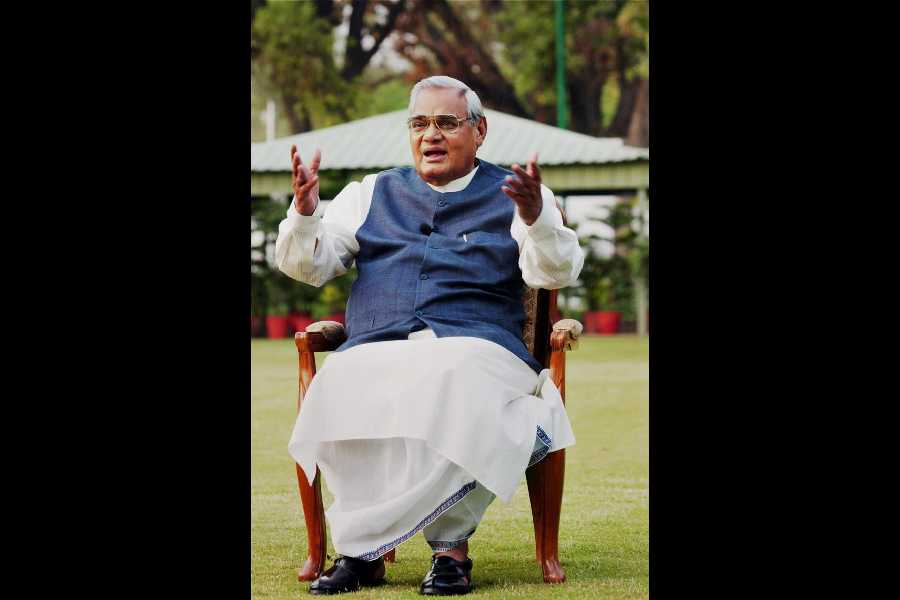
Fast forward. Fast forward. Fast forward. And stop at 2018. “Losing general practitioners (GPs) or community physicians is possibly one of the biggest losses in healthcare,” says Dr Diptendra Sarkar, a surgical oncologist and breast surgeon. We are sitting in his office at Calcutta’s IPGMER and SSKM Hospital, where he is a professor with the department of breast cancer. He continues, “If you look at global models, the skeleton of healthcare delivery is a GP. It is very unfortunate that we choose the wrong things from the West. In this case, specialisation and super specialisation.”
About a year ago, there were some incidents of angry patients going on a rampage at hospitals. There were complaints of negligence and inflated bills. Against that backdrop, speaking to The Telegraph, Dr Sarkar had said something that stuck. He had said: “A lot of this has to do with the disappearance of the neighbourhood GP. As doctors become inaccessible to the general public, and come to be creatures of specialised spaces, these problems will only increase.”
Today, he tells us what Dr Donald Weaver, his mentor from the US’s Detroit Medical University, told him some years ago. He prefaces the anecdote with the information that Professor Weaver has emotional ties with India stemming from the early 1970s when he interned with a government hospital in India and is conversant with the political as well as social changes in the country. Says Dr Sarkar, “He said he was astonished at how physicians [in India] seemed to enjoy adding 15 qualifications after their name. In the US people have only one [qualification] — MD. It is the number of years spent in training that counts.”
Dr Sarkar explains how here government policy does not focus on training. “The latest Government of India diktat is that district hospitals should be turned into PG hospitals.” His pitch rises and he thunders, “Why do you need more postgraduates and super specialists to cater to diarrhoea, asthma, hypertension, diabetes, chronic cough and fever?”
But first, when did it get to be this way? Late 1990s, says Dr Sarkar. Turn of the century says Dr Shantanu Nandy, a physician based in south Calcutta. Dr Adul Islam, a specialist physician practicing in the Ripon Street, Park Street, Park Circus areas, settles for the last five years.
And the triggers were? Dr Sarkar says the change is closely linked to corporatisation of healthcare. According to him, once healthcare ceased to be a bipartite doctor-patient arrangement and became a tripartite affair with the hospital as the most active and interested party, the denouement began. For Dr Nandy the exact moment of unspooling would be the coming into being of the Consumer Protection Act. In 1986, the Supreme Court stipulated that medical services to patients would come under the purview of this Act. “Some imperceptible shift happened then on. And today doctors are at a juncture when a patient is perceived as a potential litigator first and a patient, thereafter,” he says.
There is that thing said about absolute power corrupting absolutely. So absolute and pervasive is the new medical order, that most Indians below a certain age would not have known anything else. Those who do must strain to remember.
Sarkar speaks of the GP from his childhood days, who lived across the street. “We believed him as a doctor, but as a person before that,” he says. His own father Dr Prasanta Kumar Sarkar used to be head of the department of paediatric surgery at Calcutta Medical College. In a WhatsApp audio clip, the octogenarian who is currently ailing tells The Telegraph about two GPs who remained emblazoned in his memory — Dr Vijyendran Basak and Dr Nanigopal Ray. Says Dr Sarkar Senior in his ancient voice, trembling with emotion, “Dr Basak was very softspoken, seemed to cure his patients by his words alone. Dr Ray’s demeanour was different. He would scold his patients relentlessly, but at the end of it would not charge a penny.” By way of illustrating doctor-patient relations from his own time, he talks about a patient who came to him from the Sunderbans. “He could not afford a bed in the hospital. I had no choice but to bring him home. And after he was cured, he begged me to find him a job. I did and to my great satisfaction he is self-sufficient today.” The elder’s tone throughout the narrative is stark but not cold, he is engaged without being self-indulgent.
Dr Islam says it was natural to invite the house physician for family festivities. Dr Nandy reminds that from being closely engaged with the patient’s context, the diagnoses for ailments were more accurate, the treatment more wholistic. Each of these seasoned practitioners agree that for all the things which treatment or medicine did not or could not cure, there was a soothing stream of communication.
Says Dr Sarkar, “Today, when you have unabated fever and you are admitted to a hospital, you enter a dark tunnel. A doctor will be in attendance, and will be competent too, but it will never have the same effect as having the family physician, the physician who is an extension of your family, by your side.”
Dr Nandy tells us an anecdote from his boyhood. It seems, before every other exam he would come down with herpes, and the Madhyamik (Class X) eve was
no exception. He says, “Now I understand that it was brought on by my anxiety, but then I was an impatient patient, cantankerous from the pain. Rather audaciously I told our GP — one
Dr Mukherjee who had his chamber on Rashbehari Avenue — ‘Your medicines are absolutely useless. I am sure you cheated your way through the medical exams’.”
So many years on, Dr Nandy turns purple at the memory. “I got a good and much deserved dose from my father that day,” he laughs. Then adds, “But the good doctor laughed genially that day; he understood my discomfort.”
Today, doctor-patient run-ins assume ugly proportions. Violent proportions that can be achieved only when the other is an unknown, a stranger.
Dr Sarkar points out, “Even today, GPs functioning at the community level never face violence. Violence happens in impersonal spaces.” He, too, has an anecdote to share. Something he learnt from Dr P.K. Ray, a very senior doctor and a general practitioner from Netaji Nagar.
One time the doctor had prescribed antacid to a patient. The next day the patient returned fuming and accused him of trying to poison him. Hearing his rant, other patients gathered around. Dr Sarkar narrates, “Dr Ray told me how he asked the patient to bring him the bottle of antacid, whose contents he then proceeded to empty with, ‘Let us see who dies first.’ After some time when both parties were still alive and kicking, the crowd dissipated, as did that patient’s anger. Dr Ray told me that after that day he was never questioned by a patient again.”
Both Dr Islam and Dr Nandy talk about how each of them consciously chose to be GPs, despite their specialisations. They seem to thrive from the connect and exult in the mundane, which they say hone expertise.
Dr Nandy says how till the mid-1990s an undergraduate course in medicine involved four-and-a-half years of course work, after which one got a temporary registration number. This was followed by a year’s internship upon completing which the permanent registration number was given. Post this, if one wanted to opt for a postgraduate course, a year of housejob or practical training in a discipline of one’s choice was compulsory. “Today, the housejob is no longer mandatory,” he points out.
Speaking to people in the fraternity, we get a sense that among young doctors now, a GP is an unglamorous tag. The very sound of an alpha beta gamma specialist has a grand ring to it. But ultra ultra specialists won’t palpate, won’t ask after the colour of the stool, won’t poke and prod or wield the stetho. In this topsy-turvy world, the GP is Doctor Google.
Says Dr Islam, “Earlier people didn’t even know names of medicines. Now, by the time they come to consult us, they have already taken some over-the-counter drug. And even thereafter, they prefer to see a specialist. But the problem with that approach is — should you have a chest pain and head straight for a cardiologist, remember, his focus will be to exclude a cardiac problem and should it not be one, the treatment will end right there.”
It does not stop at that. Patients even sign themselves up for MRIs and USGs on whim. Unbridled chaos. Expensive chaos.
From Dr Sarkar we learn about the current healthcare model in the UK, where GPs are trained in the basics of gynaecology, ophthalmology, ENT, surgery and general medicine. There is a GP, who is a private practitioner, empanelled by the government for each and every zone. A patient has to go to him for treatment and only if and when he fails to diagnose the problem is the patient directed to a specialist.
The US too has started a GP grid, which works along similar lines. Dr Sarkar says, “Here too instead of producing super specialists who are not needed, we should train GPs to a broader base.”
***
As Dr Sachindranath Sen lay dying from cancer, his wife requested his old friend and classmate to pay a visit. When B.C. Ray emerged from Sen’s room, he said, “He has read his own pulse and as you know, his prognosis is infallible. He has foretold his own end.”
The pulse, the pulse, the answer for us too lies in the pulse.